Understanding Vasovagal Syncope: Causes, Symptoms, and Treatment
Vasovagal syncope, also known as neurocardiogenic syncope or reflex syncope, is a common condition that affects millions of people worldwide. In this article, we will delve into the intricate details of this disorder, exploring its causes, symptoms, and available treatment options. It is essential to understand the intricacies of vasovagal syncope to provide a comprehensive overview for those seeking knowledge about this condition.
What is Vasovagal Syncope?
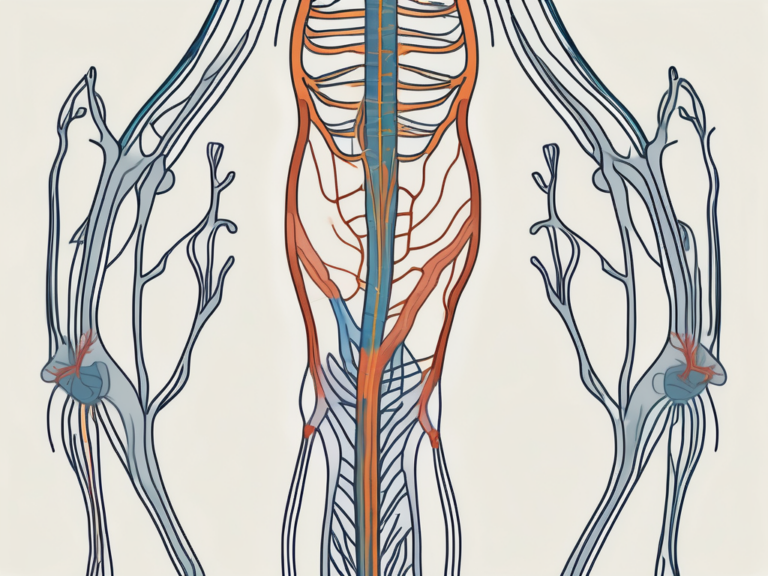
Vasovagal syncope is a transient loss of consciousness that occurs due to a sudden drop in blood pressure and heart rate. It is a reflex response triggered by the stimulation of the vagus nerve, which plays a crucial role in controlling the body’s involuntary functions. This response occurs when the body experiences certain triggers, leading to a temporary disruption in blood flow to the brain.
Vasovagal syncope is a fascinating physiological phenomenon that highlights the intricate interplay between the nervous system and cardiovascular system. When a person experiences an emotional or physical trigger, such as fear, pain, or standing up quickly, the vagus nerve is activated, causing the heart rate to slow down and blood vessels to dilate. This sudden shift in autonomic function can result in a temporary lack of oxygenated blood reaching the brain, leading to a brief loss of consciousness.
Definition and Overview
Vasovagal syncope is a type of fainting spell or fainting episode that can occur in response to emotional distress, pain, or certain situational triggers. It is characterized by a sudden loss of consciousness, often accompanied by a feeling of lightheadedness, dizziness, and weakness.
During a vasovagal syncope episode, the body’s natural response mechanisms are temporarily disrupted, causing a cascade of events that result in the individual fainting. This transient loss of consciousness is typically short-lived, with most individuals regaining full awareness within a few seconds to minutes. Understanding the physiological mechanisms underlying vasovagal syncope can empower individuals to recognize potential triggers and take appropriate steps to prevent future episodes.
Prevalence and Demographics
Vasovagal syncope is a relatively common condition, accounting for a significant proportion of fainting episodes. It is more prevalent in certain populations, such as young adults and the elderly, with a higher incidence in females compared to males. Though not life-threatening in most cases, understanding the causes and symptoms of vasovagal syncope can help individuals manage and prevent future episodes.
Research suggests that individuals with a history of vasovagal syncope may benefit from lifestyle modifications, such as staying hydrated, avoiding triggers, and practicing stress-reduction techniques. By incorporating these strategies into their daily routine, individuals can potentially reduce the frequency and severity of vasovagal syncope episodes, improving their overall quality of life.
The Physiology of Vasovagal Syncope
To comprehend the intricacies of vasovagal syncope, we must delve into the underlying physiology that drives this condition. Two primary factors contribute to syncope episodes – the role of the vagus nerve and the body’s response to stress.
Vasovagal syncope, often referred to as neurocardiogenic syncope, is a common cause of fainting episodes. It occurs when the body overreacts to certain triggers, causing a sudden drop in blood pressure and heart rate, leading to a temporary loss of consciousness. Understanding the intricate mechanisms behind this phenomenon can shed light on how to manage and prevent such episodes effectively.
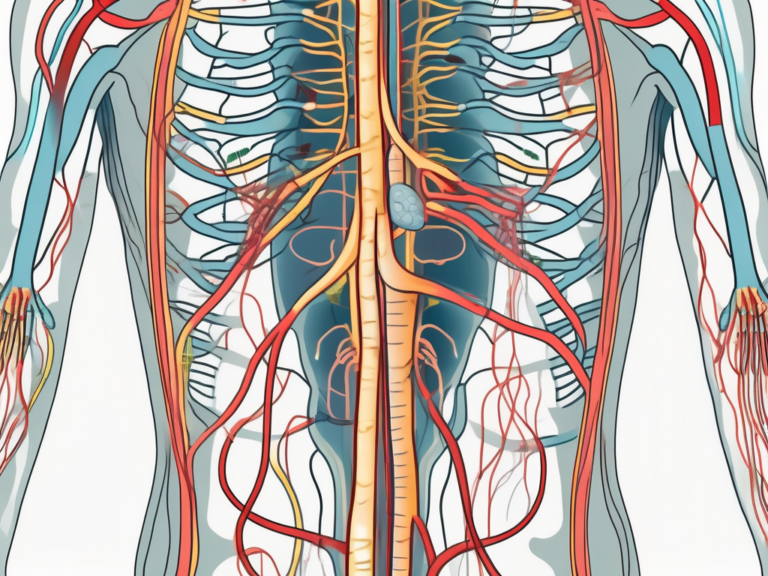
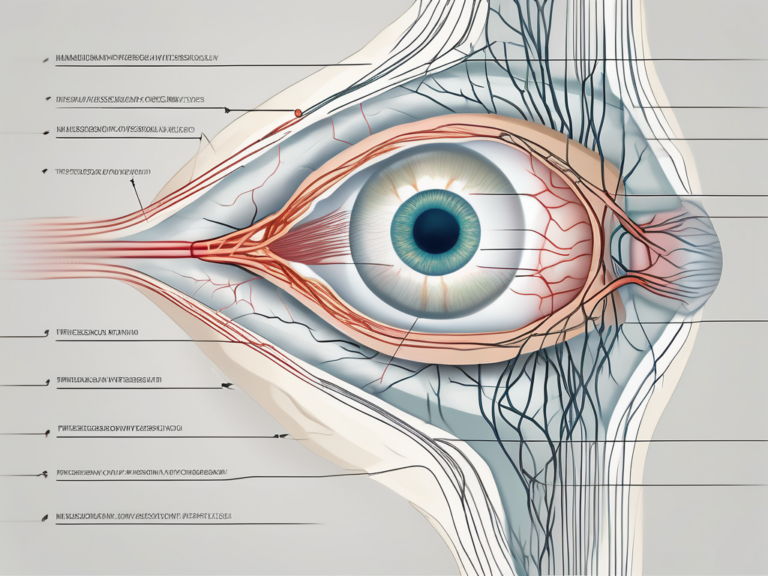
The Role of the Vagus Nerve
The vagus nerve, also known as the tenth cranial nerve, is responsible for regulating many essential bodily functions, including heart rate, blood pressure, and digestion. When stimulated, the vagus nerve triggers a complex cascade of events that lead to a temporary decrease in heart rate and a subsequent drop in blood pressure, resulting in syncope.
Furthermore, the vagus nerve plays a crucial role in the body’s parasympathetic nervous system, often referred to as the “rest and digest” system. Activation of the vagus nerve can lead to a state of relaxation and decreased physiological arousal, which can be beneficial in normal circumstances but can result in syncope when triggered excessively.
The Body’s Response to Stress
The body’s response to stress involves a remarkable interplay between the autonomic nervous system, responsible for controlling the body’s involuntary functions, and the hypothalamic-pituitary-adrenal axis, which regulates the release of stress hormones. In susceptible individuals, emotional distress, pain, or certain environmental triggers can activate this response, leading to vasovagal syncope.
Moreover, the body’s response to stress is a finely tuned mechanism designed to help individuals cope with challenging situations. However, in some cases, an exaggerated response can occur, leading to vasovagal syncope. Understanding the triggers and individual predispositions to this response is crucial in developing effective management strategies for those prone to fainting episodes.
Identifying the Causes of Vasovagal Syncope
Pinpointing the causes of vasovagal syncope is crucial for effective management and prevention. While triggers can vary from person to person, some common factors contribute to the onset of syncope episodes.
Vasovagal syncope, also known as neurocardiogenic syncope, is a common cause of fainting episodes. It occurs when there is a sudden drop in heart rate and blood pressure, leading to a temporary loss of consciousness. Understanding the mechanisms behind vasovagal syncope can help individuals recognize and manage their triggers effectively.
Common Triggers for Vasovagal Syncope
Triggers for vasovagal syncope can range from physical factors such as standing up for long periods, prolonged exposure to heat, or even the sight of blood, to emotional stressors like anxiety or fear. Identifying individual triggers is essential to minimize the occurrence of syncope episodes.
In addition to physical and emotional triggers, certain lifestyle factors can also contribute to the development of vasovagal syncope. Dehydration, lack of sleep, and excessive alcohol consumption can exacerbate symptoms and increase the risk of fainting spells. Maintaining a healthy lifestyle, including staying hydrated and getting an adequate amount of rest, can help reduce the frequency of syncope episodes.
Underlying Health Conditions
While vasovagal syncope can occur as an isolated event, it can also be associated with underlying health conditions. Certain disorders, such as heart rhythm abnormalities, structural heart diseases, or autonomic nervous system dysfunctions, can increase the likelihood of developing syncope episodes. A thorough medical evaluation is necessary to identify and manage any associated conditions.
Individuals with a history of vasovagal syncope should work closely with healthcare providers to determine the underlying causes and develop a personalized management plan. This may include lifestyle modifications, medication management, or interventions to address specific triggers. By addressing the root causes of vasovagal syncope, individuals can effectively reduce the frequency and severity of fainting episodes, improving their overall quality of life.
Recognizing the Symptoms of Vasovagal Syncope
Recognizing the symptoms of vasovagal syncope is crucial for distinguishing it from other types of fainting episodes and ensuring appropriate management. Symptoms can be divided into physical manifestations and emotional/cognitive aspects.
Vasovagal syncope is a common cause of fainting episodes and is often triggered by a sudden drop in blood pressure and heart rate, leading to a temporary reduction in blood flow to the brain. Understanding the symptoms associated with this condition can help individuals and healthcare providers identify and manage episodes effectively.
Physical Symptoms
During a vasovagal syncope episode, individuals may experience lightheadedness, dizziness, pallor, sweating, and a rapid heartbeat. These symptoms often precede the loss of consciousness, providing an early warning sign for the onset of a syncope episode.
In addition to these physical symptoms, some individuals may also report visual disturbances, such as tunnel vision or seeing spots, as well as nausea or abdominal discomfort. These additional signs can further aid in the recognition and diagnosis of vasovagal syncope.
Emotional and Cognitive Symptoms
Vasovagal syncope can also manifest with emotional and cognitive symptoms. Some individuals may experience feelings of anxiety, fear, confusion, or a sense of impending doom. While these symptoms may not be present in every case, they provide valuable insight into the underlying mechanisms of this condition.
Furthermore, individuals may also describe a feeling of warmth or flushing before losing consciousness during a vasovagal syncope episode. This sensation is attributed to the body’s autonomic response to the drop in blood pressure and can help differentiate vasovagal syncope from other causes of fainting.
Diagnostic Procedures for Vasovagal Syncope
Accurate diagnosis of vasovagal syncope is essential to rule out other potentially life-threatening causes of fainting and to guide appropriate treatment strategies. A comprehensive evaluation often involves a detailed medical history, physical examination, and specialized tests targeting syncope.
When a patient presents with symptoms suggestive of vasovagal syncope, healthcare providers embark on a journey to unravel the underlying causes of these episodes. The diagnostic process is akin to solving a complex puzzle, where each piece of information gathered contributes to painting a clearer picture of the patient’s health status.
Medical History and Physical Examination
A thorough medical history helps identify any underlying health conditions or triggers that may contribute to syncope episodes. Additionally, a physical examination can provide valuable insights into autonomic function and reveal any notable findings that warrant further investigation.
During the medical history review, healthcare professionals delve into the patient’s past medical experiences, family history, medication use, and lifestyle factors that could play a role in triggering vasovagal syncope. This detailed exploration aims to uncover any red flags or patterns that may shed light on the root cause of the fainting episodes.
Specialized Tests for Syncope
In cases where the diagnosis remains inconclusive, specialized tests may be necessary. These tests can include ambulatory electrocardiogram (ECG) monitoring, tilt table testing, or implantable loop recorders. These tests aim to capture the electrical activity of the heart and assess autonomic responses during syncope episodes.
Ambulatory ECG monitoring involves wearing a portable device that continuously records the heart’s electrical activity over an extended period, allowing healthcare providers to correlate any abnormal rhythms with syncopal events. Tilt table testing, on the other hand, involves placing the patient on a specialized table that changes positions to induce syncope under controlled conditions, aiding in the diagnosis of vasovagal syncope.
Treatment Options for Vasovagal Syncope
While vasovagal syncope generally does not require immediate medical intervention, symptomatic management and preventive strategies can help individuals maintain a good quality of life and prevent future syncope episodes.
Vasovagal syncope, also known as fainting or neurocardiogenic syncope, is a common condition characterized by a sudden loss of consciousness due to a temporary drop in blood flow to the brain. Although it can be a frightening experience, the good news is that there are various treatment options available to manage this condition effectively.
Lifestyle Changes and Home Remedies
Avoiding triggers is an essential aspect of managing vasovagal syncope. Identifying and steering clear of situations that can induce a fainting episode, such as standing for long periods, exposure to extreme heat, or emotional stress, can significantly reduce the frequency and severity of syncope episodes.
Proper hydration is another crucial factor in preventing vasovagal syncope. Ensuring an adequate intake of fluids can help maintain blood volume and prevent dehydration, which can trigger fainting episodes. Additionally, incorporating stress-reducing techniques into daily life, such as meditation, deep breathing exercises, or yoga, can help manage emotional distress effectively and reduce the likelihood of syncope episodes.
Furthermore, simple measures like changing position slowly, especially when transitioning from lying down to standing, can prevent sudden drops in blood pressure and minimize the risk of fainting. Additionally, staying cool in warm environments by wearing lightweight clothing and avoiding excessive heat exposure can also help regulate body temperature and reduce the chances of syncope.
Medications and Therapies
In certain cases, medications or therapies may be prescribed to help manage vasovagal syncope. Beta-blockers, such as propranolol or metoprolol, are commonly used to regulate heart rate and blood pressure, reducing the likelihood of syncope episodes. Fludrocortisone, a medication that helps increase blood volume, may also be prescribed in some cases. Another medication, midodrine, can help constrict blood vessels and raise blood pressure, preventing fainting episodes.
In more severe cases, where other treatment modalities have proven ineffective, cardiac pacing or other therapies targeting the autonomic nervous system may be considered. Cardiac pacing involves the implantation of a device that regulates the heart’s electrical signals, ensuring a steady heart rate and preventing sudden drops in blood pressure. These interventions should only be performed by experienced specialists after a thorough evaluation of the individual’s condition.
Surgical Interventions
In rare instances where vasovagal syncope remains refractory to other treatment options, surgical interventions may be considered. Left cardiac sympathetic denervation, a procedure that involves cutting or removing certain nerves in the chest, can help modulate the autonomic response and prevent syncope episodes. Another surgical option is the implantation of a pacemaker, which delivers electrical impulses to regulate the heart’s rhythm and prevent sudden drops in blood pressure.
It is important to note that surgical interventions are typically reserved for severe, medication-resistant cases and should be carefully considered by both the patient and their healthcare provider. These procedures require the expertise of experienced specialists and thorough evaluation to determine their appropriateness and potential benefits.
In conclusion, while vasovagal syncope can be a challenging condition to manage, there are various treatment options available to help individuals maintain a good quality of life and minimize the occurrence of syncope episodes. Lifestyle changes, medications, and in some cases, surgical interventions can all play a role in effectively managing this condition. It is crucial for individuals experiencing vasovagal syncope to work closely with their healthcare provider to determine the most suitable treatment approach based on their specific circumstances.
Living with Vasovagal Syncope
Learning to live with vasovagal syncope involves adapting to the condition and implementing effective coping strategies. Understanding triggers, managing stress, and seeking appropriate support are vital components of long-term management.
Vasovagal syncope, also known as neurocardiogenic syncope, is a condition characterized by a sudden loss of consciousness due to a temporary drop in blood flow to the brain. It can be a challenging condition to navigate, but with the right strategies in place, individuals can regain control over their lives.
Coping Strategies and Support
Individuals diagnosed with vasovagal syncope can benefit from learning coping strategies to minimize the impact of syncope episodes on their daily lives. This can include educating family and friends about the condition, carrying identification indicating a medical history of syncope, and avoiding potentially dangerous situations when symptoms manifest.
One effective coping strategy is recognizing and understanding triggers. For some individuals, certain activities or situations, such as standing for long periods, extreme heat, or emotional stress, can precipitate a syncope episode. By identifying these triggers, individuals can take proactive measures to avoid or minimize their exposure to them.
Another important aspect of coping with vasovagal syncope is managing stress. Stress can exacerbate symptoms and increase the likelihood of syncope episodes. Engaging in stress-reducing activities, such as meditation, yoga, or deep breathing exercises, can help individuals maintain a sense of calm and reduce the frequency of syncope episodes.
Seeking appropriate support is also crucial for individuals living with vasovagal syncope. Connecting with support groups or online communities can provide a sense of belonging and understanding. Sharing experiences, tips, and advice with others who are going through similar challenges can be immensely helpful in navigating the ups and downs of this condition.
Prognosis and Long-Term Management
Although vasovagal syncope can be a challenging condition to manage, the prognosis is generally positive, with most individuals experiencing a decrease in syncope frequency over time. Regular follow-up appointments with healthcare professionals and adherence to recommended treatment strategies are important for long-term management.
It is important to note that the treatment approach for vasovagal syncope may vary depending on the underlying cause and individual circumstances. Some individuals may benefit from lifestyle modifications, such as increasing fluid and salt intake, while others may require medication or even surgical interventions in severe cases.
Furthermore, staying informed about the latest research and advancements in the field of vasovagal syncope can be empowering. New treatment options and management strategies are constantly being explored, offering hope for improved quality of life for individuals living with this condition.
In conclusion, understanding the intricacies of vasovagal syncope is crucial for individuals affected by this condition, as well as their healthcare providers. By exploring the causes, symptoms, and available treatment options, we aim to provide a comprehensive overview that empowers individuals to make informed decisions about their well-being. If you suspect you may be experiencing syncope episodes, seeking medical advice and guidance is essential to ensure an accurate diagnosis and appropriate management strategies moving forward.