Understanding the Perineal Nerve: Functions and Disorders
The perineal nerve is a crucial component of the peripheral nervous system, playing a significant role in various sensory and motor functions. This article aims to provide a comprehensive understanding of the anatomy, functions, common disorders, treatment options, prevention strategies, and future research directions pertaining to the perineal nerve.
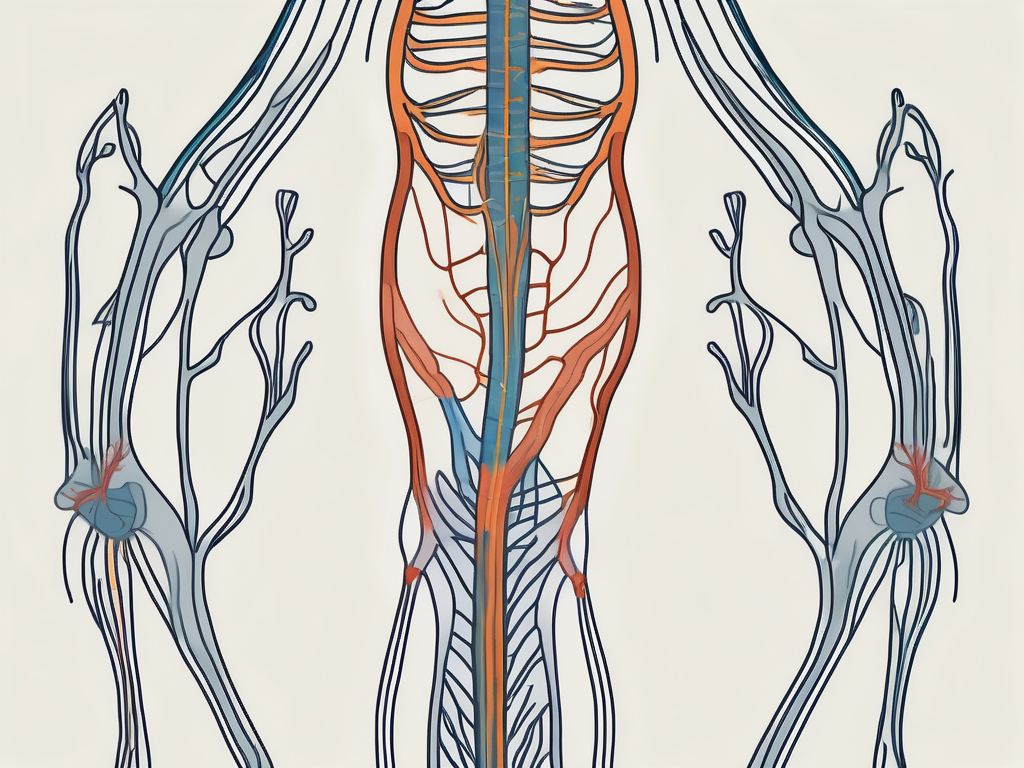
Anatomy of the Perineal Nerve
Before delving into the functions and disorders, it is essential to grasp the intricate anatomy of the perineal nerve. This nerve is a branch of the sacral plexus, arising primarily from the S2, S3, and S4 nerve roots. Its location and structure make it an integral part of the lower extremity’s innervations.
Location and Structure
The perineal nerve courses through the pelvis, traveling alongside the sacrospinous ligament and the sacrotuberous ligament. It then enters the gluteal region, supplying various muscles, including the gluteus maximus and the hip joint’s external rotators.
Descending further, the perineal nerve extends into the posterior thigh, supplying the biceps femoris and other hamstring muscles. Finally, it terminates in the perineum, where it plays a vital role in innervating the external genitalia and perineal muscles.
Within the perineum, the perineal nerve branches out extensively, forming connections with the pudendal nerve, which is crucial for the sensation and motor function of the pelvic floor muscles. Additionally, it communicates with the posterior femoral cutaneous nerve, contributing to the sensory innervation of the lower limb.
Connection to Other Nerves
The perineal nerve has extensive communication with other nerves within the sacral plexus. For instance, it forms connections with the pudendal nerve, which plays a dominant role in the innervation of the perineum. These intricate interconnections ensure the proper functioning of the lower limb and pelvic region.
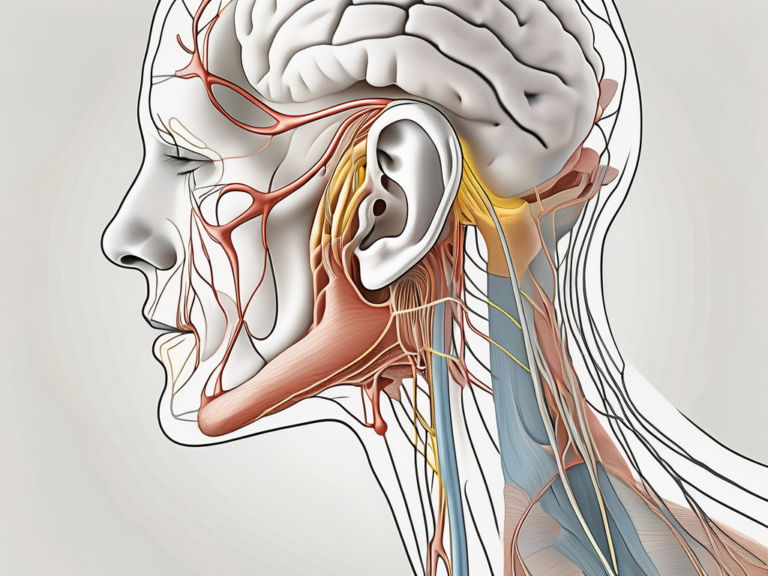
Functions of the Perineal Nerve
The perineal nerve performs a wide array of functions, predominantly related to sensory perception and motor control. Understanding these functions is crucial in comprehending the impact of perineal nerve disorders.
The perineal nerve, a branch of the pudendal nerve, is a vital component of the sacral plexus. It arises from the S2-S4 nerve roots and travels through the pelvis, providing innervation to various structures in the perineum and lower extremities.
Role in Sensory Perception
One of the primary functions of the perineal nerve is sensory perception in the lower extremities. It provides sensory feedback from the perineum, external genitalia, and the posterior thigh. This information is critical for maintaining balance, proprioception, and overall body awareness.
In addition to its role in sensory perception, the perineal nerve also carries sensory fibers that contribute to sexual function. The nerve endings in the external genitalia play a crucial role in sexual arousal and pleasure, highlighting the intricate connection between neurological function and sexual health.
Influence on Motor Control
Besides sensory perception, the perineal nerve plays a crucial role in motor control. It innervates several muscles, including the external anal sphincter, levator ani, and the perineal muscles. By coordinating the contraction and relaxation of these muscles, the perineal nerve enables proper defecation, micturition, and sexual function.
The perineal nerve’s motor function extends beyond basic bodily functions, contributing to the stability of the pelvic floor. Proper functioning of the perineal muscles is essential for supporting pelvic organs, maintaining continence, and facilitating efficient movement.
Common Disorders Affecting the Perineal Nerve
Despite its vital functions, the perineal nerve is susceptible to various disorders that can significantly impact an individual’s quality of life. Understanding the causes, symptoms, and diagnosis of these disorders is crucial for effective management.
The perineal nerve, a branch of the pudendal nerve, plays a crucial role in innervating the perineum, which includes the external genitalia and the anal region. Any disruption to its function can result in debilitating consequences for individuals, affecting not only their physical well-being but also their emotional and psychological health.
Causes and Risk Factors
Perineal nerve disorders can arise from various underlying causes and risk factors. Traumatic injuries, such as pelvic fractures sustained in accidents or falls, can directly impinge upon or damage the perineal nerve, leading to neuropathic pain and sensory disturbances. Additionally, prolonged compression or entrapment of the nerve, as seen in cyclists spending long hours on narrow bicycle seats or individuals with sedentary occupations requiring prolonged sitting, can contribute to nerve dysfunction and chronic discomfort.
Furthermore, medical conditions such as diabetes, which is known to cause peripheral neuropathy, can also affect the perineal nerve. The metabolic disturbances associated with diabetes can result in nerve damage over time, exacerbating symptoms and complicating treatment approaches for perineal nerve disorders.
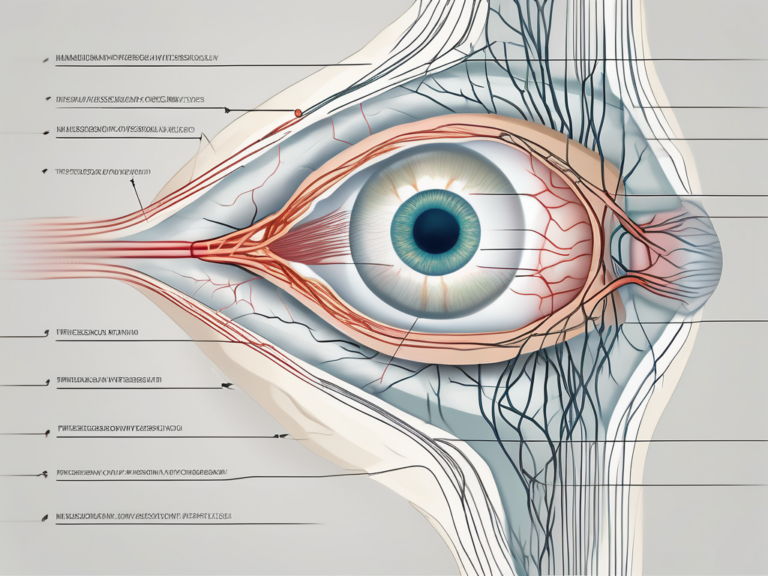
Symptoms and Diagnosis
Perineal nerve disorders present with an array of symptoms, which can vary depending on the specific condition. Common symptoms include numbness or tingling in the perineum or the posterior thigh, weakened perineal muscles leading to urinary or fecal incontinence, and sexual dysfunction affecting intimacy and quality of life. Individuals may also experience shooting or burning pain in the affected area, further adding to their discomfort and distress.
A thorough clinical examination, conducted by a healthcare professional with expertise in neurology or urology, is essential for evaluating the extent of perineal nerve dysfunction. In addition to a detailed medical history and physical assessment, diagnostic tests such as electromyography (EMG) and nerve conduction studies (NCS) may be employed to assess nerve conduction velocity and muscle response, aiding in accurately diagnosing perineal nerve disorders and guiding appropriate treatment strategies.
Treatment Options for Perineal Nerve Disorders
Effective management of perineal nerve disorders requires a multidimensional approach, tailored to the individual’s specific condition and needs. Treatment options may include non-surgical interventions or surgical procedures.
Perineal nerve disorders can significantly impact an individual’s quality of life, leading to symptoms such as pain, numbness, and tingling in the perineal region. It is essential to address these symptoms promptly to prevent further complications and improve overall well-being.
Non-Surgical Interventions
In many cases, non-surgical interventions can alleviate the symptoms associated with perineal nerve disorders. These may include physical therapy, which aims to strengthen the perineal muscles and improve overall nerve functioning. Physical therapists can create customized exercise regimens to target specific areas of weakness or dysfunction, promoting nerve health and mobility.
Furthermore, lifestyle modifications, such as ergonomic adjustments and activity modifications, may also play a crucial role in managing perineal nerve disorders. By identifying and avoiding triggers that exacerbate symptoms, individuals can better control their condition and prevent flare-ups.
Surgical Procedures
In instances where non-surgical interventions fail to adequately address the condition, surgical procedures may be recommended. Surgical interventions may involve nerve repair or decompression to alleviate nerve compression or remove scar tissue. These surgeries are often performed by specialized surgeons, such as peripheral nerve surgeons, to optimize outcomes.
Prior to undergoing surgery, individuals will undergo a comprehensive evaluation to determine the most appropriate surgical approach for their specific condition. This evaluation may include diagnostic imaging studies, nerve conduction tests, and consultations with a multidisciplinary team of healthcare providers to ensure a comprehensive and personalized treatment plan.
Prevention and Management of Perineal Nerve Disorders
While not all perineal nerve disorders can be prevented, certain strategies can help reduce the risk of developing these conditions or manage existing ones.
Perineal nerve disorders can be debilitating, impacting daily activities and quality of life. Therefore, adopting preventive measures and effective management strategies is essential for individuals at risk or already experiencing symptoms.
Lifestyle Modifications
Maintaining a healthy lifestyle is crucial in preventing perineal nerve disorders. Regular exercise, maintaining a healthy weight, and avoiding prolonged sitting or repetitive activities that may compress the nerve can greatly reduce the risk. Additionally, maintaining proper posture and utilizing ergonomic equipment can aid in mitigating the risk of nerve compression.
Furthermore, incorporating stress-reducing activities such as yoga or meditation can help alleviate tension in the pelvic area, reducing the likelihood of nerve compression and related symptoms.
Physical Therapy and Exercises
Physical therapy and targeted exercises can play a significant role in managing perineal nerve disorders. A tailored exercise program focusing on strengthening the perineal muscles, improving flexibility, and enhancing overall nerve functioning can aid in symptom relief and functional improvement.
Engaging in pelvic floor exercises, such as Kegels, can specifically target the muscles surrounding the perineal area, promoting better nerve function and circulation. Additionally, activities like cycling or swimming can help improve blood flow to the perineum, supporting nerve health and reducing discomfort.
Future Research Directions in Perineal Nerve Health
As our understanding of the perineal nerve and its disorders continues to evolve, ongoing research is aimed at developing new treatment modalities and addressing unanswered questions in the field.
Emerging Therapies
Ongoing research endeavors are exploring emerging therapies, such as regenerative medicine, novel surgical techniques, and advanced neurostimulation approaches to improve the outcomes for individuals with perineal nerve disorders. These advancements hold promise in alleviating symptoms and improving the overall quality of life for affected individuals.
Regenerative medicine, for instance, involves the use of stem cells or tissue engineering to repair or replace damaged perineal nerve tissue. This innovative approach aims to restore normal nerve function and promote regeneration, offering a potential breakthrough in the treatment of perineal nerve disorders.
In addition to regenerative medicine, novel surgical techniques are being investigated to address perineal nerve disorders. Surgeons are exploring minimally invasive procedures that can precisely target the affected area, minimizing trauma and reducing the risk of complications. These techniques aim to optimize surgical outcomes and improve patient recovery.
Furthermore, advanced neurostimulation approaches are being studied as potential therapeutic options for perineal nerve disorders. Neurostimulation involves the use of electrical impulses to modulate nerve activity and alleviate symptoms. Researchers are exploring various neurostimulation techniques, including spinal cord stimulation and peripheral nerve stimulation, to determine their efficacy and safety in managing perineal nerve disorders.
Unanswered Questions in Perineal Nerve Research
Despite significant strides in perineal nerve research, there remain several unanswered questions. Clarifying the optimal management strategies, understanding the long-term outcomes of different treatment interventions, and further elucidating the underlying pathophysiology of perineal nerve disorders are vital areas of research that hold potential for future breakthroughs.
One of the key unanswered questions in perineal nerve research is the optimal management strategy for different types of perineal nerve disorders. While current treatment options exist, there is a need for further research to determine the most effective approach for each specific condition. This includes identifying the appropriate combination of therapies, such as medication, physical therapy, and surgical interventions, to achieve optimal outcomes.
Additionally, understanding the long-term outcomes of different treatment interventions is crucial for evaluating their effectiveness and guiding clinical decision-making. Longitudinal studies that follow patients over an extended period are needed to assess the durability of treatment effects, potential complications, and overall patient satisfaction.
Furthermore, further elucidating the underlying pathophysiology of perineal nerve disorders is essential for developing targeted therapies. By unraveling the mechanisms that contribute to nerve dysfunction, researchers can identify novel therapeutic targets and develop more tailored treatment approaches.
In conclusion, the perineal nerve plays a pivotal role in various sensory and motor functions within the lower extremities and pelvic region. Understanding the anatomy, functions, common disorders, treatment options, prevention strategies, and future research directions pertaining to the perineal nerve is crucial for healthcare professionals and individuals affected by these conditions. By staying abreast of the latest advancements and disseminating accurate information, we can continue to enhance patient care and improve outcomes in perineal nerve health.