The Comprehensive Guide to the Mandibular Nerve
The mandibular nerve is a crucial component of the trigeminal nerve system, responsible for providing sensory and motor innervation to the lower face, chin, lower lip, and the majority of the oral cavity. Understanding the anatomy, functions, disorders, diagnostic procedures, and treatment options associated with the mandibular nerve is essential for healthcare professionals working in the field of oral and maxillofacial health. In this comprehensive guide, we will explore the intricacies of the mandibular nerve, its related disorders, diagnostic approaches, as well as prevention and management strategies.
Understanding the Mandibular Nerve
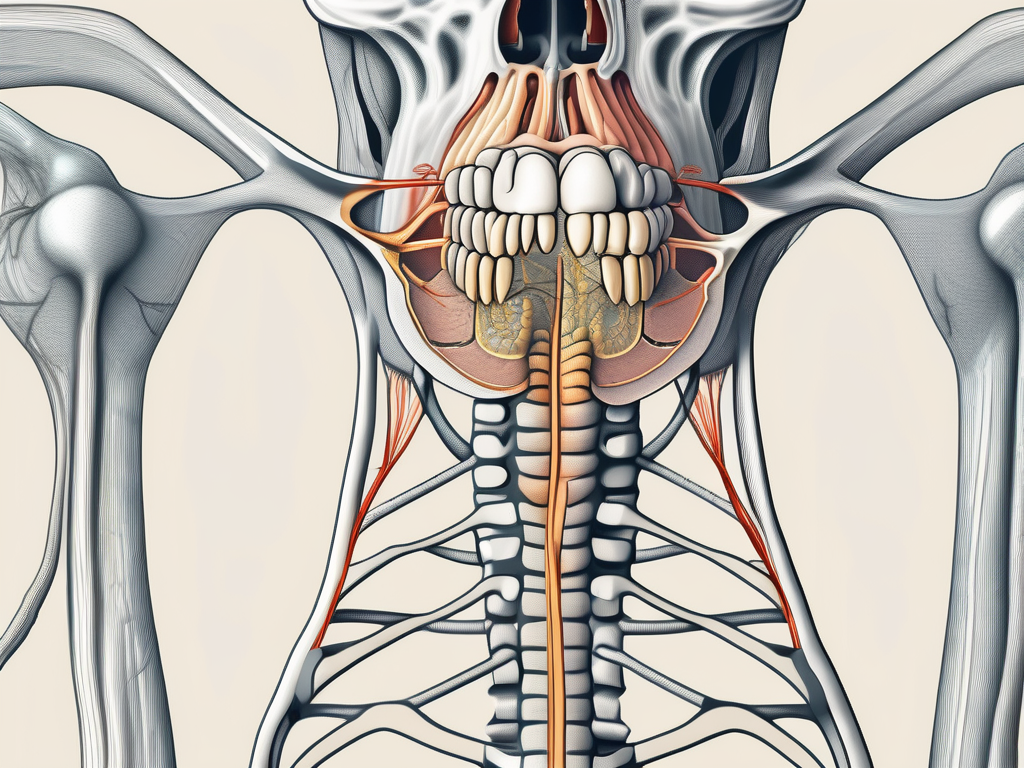
Anatomy of the Mandibular Nerve
The mandibular nerve, also known as the V3 branch of the trigeminal nerve, is a fascinating structure that plays a crucial role in transmitting sensory information from the face to the brain. Originating from the trigeminal ganglion, a cluster of nerve cell bodies located within the cranial cavity, the mandibular nerve embarks on a remarkable journey through the intricate pathways of the skull.
As it ventures out of the cranial cavity, the mandibular nerve gracefully exits through the foramen ovale, a bony opening in the base of the skull. This exit point serves as a gateway for the nerve to embark on its mission of providing sensory and motor innervation to various regions of the face.
Once outside the skull, the mandibular nerve branches out into three primary divisions, each with its own unique responsibilities. These divisions are like the branches of a mighty tree, reaching out to different areas of the face, ensuring that no sensation goes unnoticed.
- The anterior division, the first branch of the mandibular nerve, is responsible for providing sensory innervation to the lower lip and chin. It is through this division that we are able to feel the gentle touch of a loved one’s hand on our chin or the warmth of a cup of tea against our lower lip.
- The middle division, like a caring guardian, extends its sensory fibers to the cheeks and the temporomandibular joint. This division allows us to experience the sensation of a gentle breeze against our cheeks or the subtle movements of our jaw as we speak.
- The posterior division, the final branch of the mandibular nerve, ventures even further, supplying sensory innervation to the external ear and scalp. It is through this division that we are able to feel the tickle of a gentle breeze against our ears or the comforting touch of a hairbrush against our scalp.
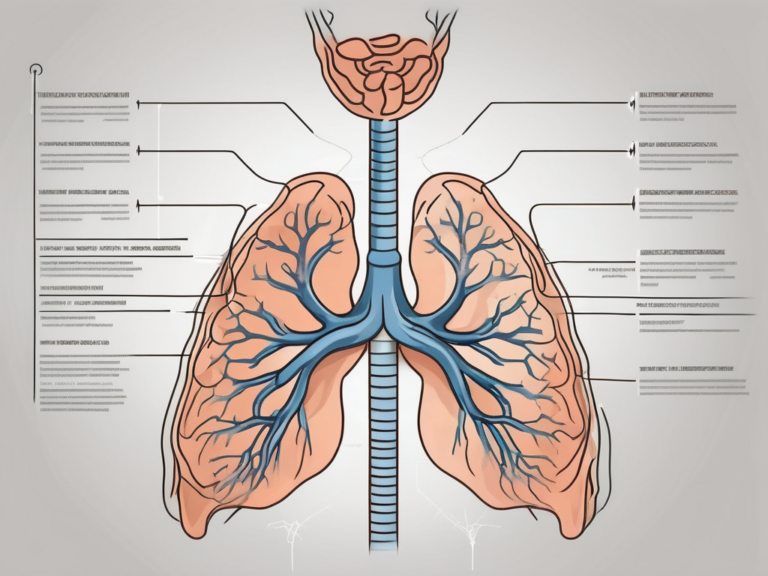
Functions of the Mandibular Nerve
The mandibular nerve, with its intricate network of sensory fibers, is a key player in various critical functions of the oral cavity. It serves as the messenger, transmitting sensory signals from the lower face, chin, and lower lip to the brain, allowing us to perceive touch, temperature, pressure, and pain in these areas.
But the mandibular nerve’s responsibilities do not end there. It also takes charge of the muscles involved in chewing, ensuring that the process of mastication is carried out with precision and coordination. Without the mandibular nerve, the simple act of chewing our food would be a challenging task.
The Mandibular Nerve and the Trigeminal Nerve System
While the mandibular nerve is an impressive structure on its own, it is intricately connected to the overall trigeminal nerve system. The trigeminal nerve, often referred to as the V cranial nerve, is a complex network responsible for providing sensation to the entire face, as well as motor innervation to the muscles involved in facial expression and chewing.
Disorders affecting the mandibular nerve can have far-reaching implications on the overall trigeminal nerve system, leading to a wide range of symptoms and functional limitations. From facial pain to difficulty in chewing, these disorders can significantly impact an individual’s quality of life.
Understanding the intricacies of the mandibular nerve and its relationship with the trigeminal nerve system is a fascinating journey into the world of human anatomy. It reminds us of the remarkable complexity and interconnectedness of our bodies, and the importance of these intricate structures in our everyday lives.
Disorders Related to the Mandibular Nerve
Trigeminal Neuralgia
Trigeminal neuralgia, also known as tic douloureux, is a debilitating condition characterized by severe facial pain, often triggered by facial movements or even gentle touch. The condition primarily affects the mandibular nerve and is typically caused by compression or irritation of the nerve root. Trigeminal neuralgia can significantly impact a patient’s quality of life, causing excruciating pain and limitations in everyday activities such as eating and speaking.
Patients with trigeminal neuralgia often describe the pain as sharp, shooting, or like an electric shock, affecting specific areas of the face innervated by the mandibular nerve. The episodes of pain can be brief but intense, leading to a fear of triggering an attack with simple actions like brushing teeth or applying makeup. Treatment options for trigeminal neuralgia range from medications to surgical interventions, aiming to alleviate pain and improve the patient’s overall well-being.
Mandibular Nerve Neuropathy
Mandibular nerve neuropathy refers to damage or dysfunction of the mandibular nerve, resulting in abnormal sensations, numbness, or pain in the lower face and oral cavity. This condition can be caused by various factors, including trauma, infection, nerve compression, or systemic diseases such as diabetes. Prompt diagnosis and appropriate management are essential to prevent further complications and alleviate symptoms.
In cases of mandibular nerve neuropathy, patients may experience tingling or burning sensations in the lower face, along with muscle weakness that can affect chewing and facial expressions. Management of this condition involves addressing the underlying cause, such as treating infections or providing physical therapy to improve nerve function and reduce discomfort.
Mandibular Nerve Compression
Mandibular nerve compression occurs when the nerve is compressed or trapped by surrounding structures, leading to impaired sensory or motor function. Common causes of compression include dental abscesses, tumors, or structural abnormalities within the skull or jaw. Early identification and intervention are crucial to prevent permanent damage and alleviate symptoms.
Compression of the mandibular nerve can result in symptoms such as numbness in the lower face, difficulty opening or closing the mouth, and pain that radiates to the ear or temple. Treatment for mandibular nerve compression may involve addressing the underlying cause, such as removing tumors or abscesses, or surgical procedures to relieve pressure on the nerve and restore normal function.
Diagnostic Procedures for Mandibular Nerve Issues
Clinical Examination
A thorough clinical examination is the initial step in diagnosing mandibular nerve issues. Healthcare professionals will carefully evaluate the patient’s symptoms, perform a comprehensive neurological examination, and review the patient’s medical history. Special attention will be given to areas of reduced sensation or abnormal motor function in the lower face, chin, and oral cavity.
During the clinical examination, healthcare providers may also assess the patient’s reflexes, muscle strength, and coordination to further evaluate the extent of mandibular nerve involvement. Additionally, detailed sensory testing may be conducted to pinpoint specific areas of altered or diminished sensation, helping to localize the site of nerve dysfunction.
Imaging Techniques
Imaging techniques such as magnetic resonance imaging (MRI) and computed tomography (CT) scans can provide valuable insights into the anatomical structures surrounding the mandibular nerve. These non-invasive imaging modalities help identify potential causes of nerve compression or structural abnormalities, aiding in accurate diagnosis and treatment planning.
Furthermore, advanced imaging technologies like diffusion-weighted imaging (DWI) and magnetic resonance neurography (MRN) offer enhanced visualization of nerve tissue and can detect subtle changes in nerve morphology or signal intensity. These specialized imaging modalities play a crucial role in identifying nerve compression from adjacent structures or lesions along the nerve pathway.
Electrophysiological Testing
Electrophysiological testing, including nerve conduction studies and electromyography, can assess the overall function and integrity of the mandibular nerve. These tests measure the electrical activity within the nerve fibers and associated muscles, aiding in the diagnosis and localization of specific nerve pathologies.
In addition to traditional nerve conduction studies, newer techniques such as blink reflex testing and quantitative sensory testing (QST) may be utilized to evaluate the sensory and motor functions of the mandibular nerve more comprehensively. These specialized tests provide valuable information about nerve excitability, conduction velocities, and sensory thresholds, contributing to a more detailed understanding of the underlying nerve pathology.
Treatment Options for Mandibular Nerve Disorders
Dealing with mandibular nerve disorders can be a challenging and painful experience for many individuals. Fortunately, there are various treatment options available to help manage the symptoms and improve quality of life. In addition to the traditional medication therapies and surgical interventions, there are other avenues worth exploring to find relief and comfort.
Medication Therapies
In many cases, medications such as anticonvulsants, tricyclic antidepressants, and muscle relaxants can effectively alleviate pain and reduce symptoms associated with mandibular nerve disorders. However, it is essential to tailor the medication regimen to each patient’s specific condition and closely monitor for potential side effects. Finding the right balance of medications can make a significant difference in managing the pain and discomfort caused by the nerve disorder.
Surgical Interventions
In severe or refractory cases, surgical interventions may be necessary to alleviate pressure or repair damaged nerve structures. Surgical options may include decompression procedures, nerve repair, or even the removal of tumors or dental abscesses that may be compressing the nerve. It is important to consult with a specialist to determine the appropriate surgical approach based on the underlying cause and the patient’s overall health status. Surgery can offer a more permanent solution for those who have exhausted other treatment options.
Alternative Treatments
In addition to conventional medical and surgical interventions, some patients may find relief through alternative treatments such as acupuncture, physical therapy, or relaxation techniques. These alternative treatments focus on holistic approaches to healing and may provide additional benefits beyond symptom management. While these approaches may offer symptomatic relief for some individuals, it is crucial to discuss their potential benefits and limitations with healthcare professionals. Exploring alternative treatments can be a valuable complement to traditional therapies in the management of mandibular nerve disorders.
Prevention and Management of Mandibular Nerve Disorders
Lifestyle Modifications
Adopting a healthy lifestyle can contribute significantly to the prevention and management of mandibular nerve disorders. This includes maintaining good oral hygiene, avoiding excessive stress, and following a balanced diet rich in essential nutrients. Additionally, avoiding habits such as teeth grinding or clenching can help minimize the risk of nerve compression and related complications.
Good oral hygiene practices, such as regular brushing and flossing, are essential for maintaining the health of the mandibular nerve. By keeping the teeth and gums clean, the risk of infections and inflammation that can affect the nerve is reduced. Furthermore, practicing stress management techniques, such as meditation or exercise, can help alleviate tension in the jaw muscles and prevent nerve compression.
Regular Check-ups and Early Detection
Regular dental check-ups and visits to healthcare professionals specialized in oral health are essential for early detection and management of mandibular nerve disorders. Routine examinations can identify potential risk factors, offer guidance regarding appropriate oral hygiene practices, and provide timely interventions to prevent the progression of nerve-related issues.
During dental check-ups, dentists can perform a thorough examination of the jaw and surrounding structures to detect any signs of nerve disorders. They may also use diagnostic imaging techniques, such as X-rays or CT scans, to get a detailed view of the mandibular nerve and assess its condition. Early detection allows for prompt treatment and can help prevent further damage to the nerve.
Coping Mechanisms and Support Systems
Dealing with the challenges posed by mandibular nerve disorders can be mentally and emotionally demanding. Engaging in support networks, seeking counseling, or joining support groups can help patients and their families cope with the associated physical and emotional burdens. Healthcare professionals can also provide guidance and resources to facilitate the overall well-being of individuals affected by these conditions.
Support systems play a crucial role in helping individuals with mandibular nerve disorders navigate the complexities of their condition. Support groups provide a safe space for patients to share their experiences, exchange coping strategies, and find emotional support from others who understand their challenges. Additionally, counseling services can help individuals develop effective coping mechanisms and manage the psychological impact of living with a nerve disorder.
In conclusion, understanding the complexities of the mandibular nerve is paramount for healthcare professionals involved in the diagnosis, treatment, and management of various oral health conditions. By recognizing the anatomy, functions, disorders, diagnostic procedures, and treatment options associated with the mandibular nerve, dental and medical professionals can ensure the provision of comprehensive and effective care to individuals with these conditions. Remember, seek professional advice for accurate diagnosis and tailored treatment plans, as this comprehensive guide is intended for informational purposes only and not as medical advice.